Blog
What Does a Decompressed Gallbladder on a CT Scan Mean? Unraveling the Mystery
Introduction: Why Should You Care About a Decompressed Gallbladder?
Have you ever glanced at a CT scan report and stumbled across the term “decompressed gallbladder”? If so, you might be wondering: What does this mean, and should I be worried? A decompressed gallbladder on a CT scan can sound alarming, but it’s often a normal finding—or it could signal an underlying issue. In this article, we’ll break down what a decompressed gallbladder is, why it appears on a CT scan, its potential causes, and what you should do next. Whether you’re a patient seeking answers or simply curious about gallbladder health, let’s dive into this medical mystery together!
Understanding the Gallbladder: A Tiny Organ with a Big Role
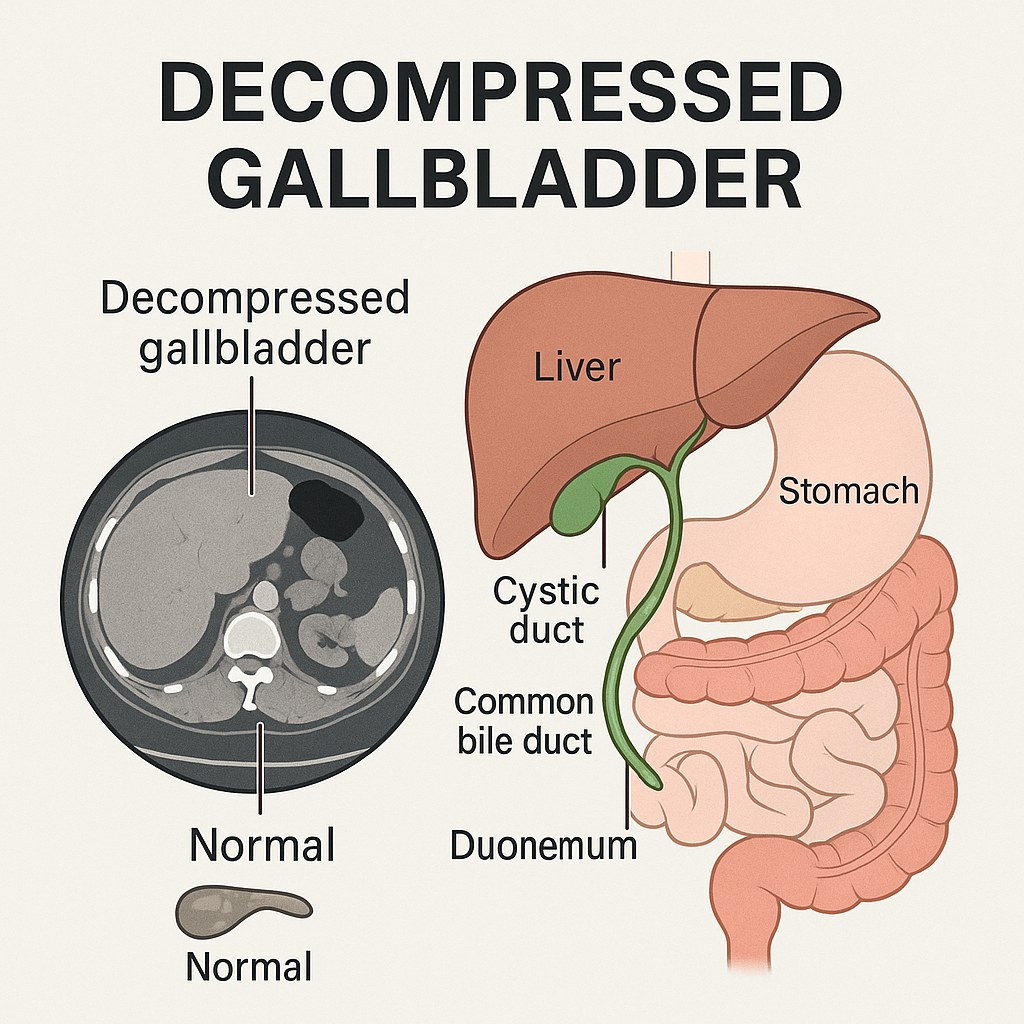
Before we explore a decompressed gallbladder, let’s ask: What does the gallbladder do? This small, pear-shaped organ, tucked beneath your liver, stores bile—a digestive fluid produced by the liver to break down fats in your small intestine. After you eat, the gallbladder contracts, releasing bile to aid digestion, then refills between meals. This natural cycle of expanding and contracting is key to its function.
On a CT scan, a “decompressed” gallbladder means it appears shrunken or collapsed, with a smaller lumen (inner space) than expected. But is this always a cause for concern? Let’s find out.
What Is a Decompressed Gallbladder on a CT Scan?
A decompressed gallbladder on a CT scan indicates that the organ is contracted, often because it has recently released bile. This can happen naturally after eating, as the gallbladder empties to help digest fats. However, a decompressed gallbladder can also appear in certain medical conditions, some benign and others more serious.
Key Characteristics on a CT Scan:
- Small Lumen: The gallbladder appears shrunken, with little to no bile visible.
- Thickened Walls: In some cases, the walls may appear thickened, especially if inflammation or gallstones are present.
- Associated Findings: Air, fluid, or gallstones may be visible, depending on the cause.
Why might a radiologist note a decompressed gallbladder? Is it always a red flag, or could it be a normal snapshot of your digestive process? Let’s explore the causes to find out.
Causes of a Decompressed Gallbladder: Normal or Not?
A decompressed gallbladder can result from both normal physiological processes and pathological conditions. Here are the main causes:
Normal Causes
- Post-Meal Contraction: After eating, the gallbladder contracts to release bile, appearing decompressed on a CT scan. If you ate a few hours before the scan, this is likely normal.
- Fasting Variability: Prolonged fasting can sometimes lead to a partially contracted gallbladder, though it’s typically less pronounced.
Abnormal Causes
- Gallstones (Cholelithiasis): Gallstones can block the cystic duct, preventing bile from filling the gallbladder, causing it to shrink. This is a common cause of a decompressed gallbladder.
- Chronic Cholecystitis: Long-term inflammation from gallstones can lead to scarring, thickening of the gallbladder walls, and a chronically contracted state.
- Gallstone Ileus: Large gallstones may escape through a fistula, causing bowel obstruction and a decompressed gallbladder.
- Perforation or Leakage: A perforated gallbladder, often due to severe cholecystitis, can result in bile leakage and a decompressed appearance.
- Porcelain Gallbladder: Chronic irritation may cause calcium deposits, leading to a hardened, shrunken gallbladder.
- Parastomal Herniation: Rarely, the gallbladder may herniate into a stoma, appearing decompressed on imaging.
Which of these causes resonates with your situation? Have you experienced symptoms like abdominal pain or nausea that might hint at an underlying issue?
Symptoms: When Should You Be Concerned?
A decompressed gallbladder doesn’t always cause symptoms, especially if it’s a normal post-meal contraction. However, when associated with conditions like gallstones or cholecystitis, you might notice:
- Right Upper Quadrant Pain: A dull or sharp pain under your right ribs, often worsening after fatty meals.
- Nausea and Vomiting: Common in acute or chronic gallbladder issues.
- Bloating or Indigestion: Difficulty digesting greasy or spicy foods.
- Jaundice: Yellowing of the skin or eyes if bile ducts are blocked.
- Fever or Chills: Suggestive of infection or perforation in severe cases.
If your CT scan shows a decompressed gallbladder but you have no symptoms, it may not require immediate action. But if you’re experiencing pain or digestive issues, what should you do next?
Diagnosing a Decompressed Gallbladder: Beyond the CT Scan
A CT scan is just one piece of the puzzle. Why might your doctor order additional tests? Because a decompressed gallbladder can be tricky to interpret, and other imaging or lab tests can clarify the cause.
Complementary Diagnostic Tools:
- Ultrasound: The gold standard for gallbladder imaging, ultrasound is more sensitive than CT for detecting gallstones and wall thickening. It can also assess gallbladder function dynamically.
- HIDA Scan: This nuclear medicine test evaluates gallbladder function by tracking bile flow. A non-visualized gallbladder may indicate obstruction or dysfunction.
- MRI/MRCP: Useful for detailed views of the biliary ducts, especially if gallstones or blockages are suspected.
- Blood Tests: Elevated liver enzymes, bilirubin, or white blood cell counts can signal infection, obstruction, or inflammation.
Have you had other tests alongside your CT scan? How might they help your doctor piece together the full picture?
Treatment Options: What Happens Next?
The treatment for a decompressed gallbladder depends on its cause. If it’s a normal finding post-meal, no action is needed. But if an underlying condition is present, options include:
- Watchful Waiting: For asymptomatic gallstones or mild cases, monitoring may be sufficient.
- Medications: Drugs to dissolve gallstones are rarely used due to slow results and recurrence risk.
- Cholecystectomy: Surgical removal of the gallbladder is the standard treatment for symptomatic gallstones or cholecystitis. Laparoscopic surgery is minimally invasive and common.
- ERCP: For bile duct blockages, endoscopic retrograde cholangiopancreatography can remove stones.
- Percutaneous Drainage: In severe cases like perforation, a tube may be inserted to drain bile.
What factors might influence your doctor’s recommendation? Could lifestyle changes, like a low-fat diet, play a role in managing symptoms?
Preventing Gallbladder Issues: Can You Stay Ahead?
Can you reduce the risk of gallbladder problems? While some factors like genetics are out of your control, lifestyle changes can help:
- Healthy Diet: Limit fatty and processed foods to reduce gallstone formation.
- Maintain a Healthy Weight: Obesity increases gallstone risk, but avoid rapid weight loss, which can also trigger issues.
- Stay Active: Regular exercise may lower the risk of gallbladder disease.
What small changes could you make today to support your gallbladder health?
Conclusion: Taking Charge of Your Gallbladder Health
A decompressed gallbladder on a CT scan can be a normal finding or a clue to an underlying issue like gallstones or cholecystitis. By understanding its causes, symptoms, and diagnostic steps, you’re better equipped to discuss your scan results with your doctor. Have you experienced symptoms that might point to gallbladder trouble? Are you ready to explore further tests or lifestyle changes to stay healthy? For more information, check out this trusted resource from Johns Hopkins Medicine. Share your thoughts or questions in the comments below!